Trusted by:
0
Major League Sports Teams
0
Colleges + Universities
0
Units in the Field

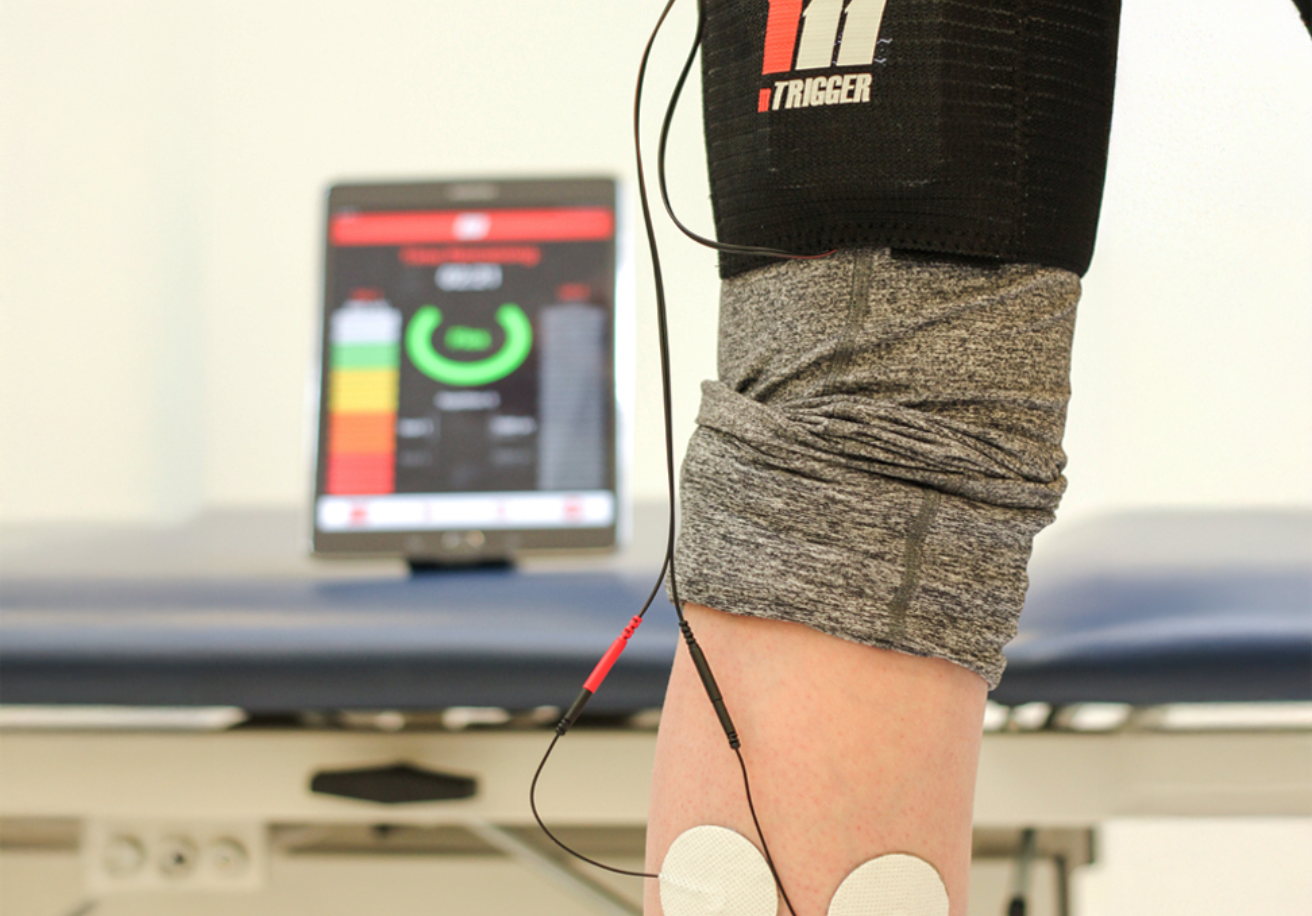
mTrigger Biofeedback
Easy-to-use sEMG (surface electromyography) biofeedback
Track muscle activation in real time with wireless sEMG biofeedback. Quick setup, simple app, powerful results.
Built by clinicians, for clinicians
Designed by rehab professionals to meet the real needs of physical therapy and performance training.
Make therapy efficient and engaging
Turn exercises into interactive sessions. Help patients stay motivated and track progress easily.
Best tools for better outcomes
mTrigger helps drive faster, more effective rehab by making muscle activation visible and measurable.

LEVEL UP YOUR REHAB PRACTICE
Quantify deficits, re-enforce proper movement patterns, and track progress.
Stand out as a fun, high-tech practice.

MAXIMIZE MUSCLE ACTIVATION
Improve muscle accuracy, effort, and patient compliance.
Expect better outcomes and make the most of every rep.

CREATE AH-HA MOMENTS
Improve decision-making with real-time data. Optimize motor programming with immediate visual feedback.
Help patients enjoy exercise.

PELVIC FLOOR HEALTH
Biofeedback can be used for regaining strength in the pelvic floor.
Sensors are placed on the abdomen and on the pelvic floor muscles muscles used during urination and bowel movements. In some cases, pelvic probes may be used.
Biofeedback simply picks up on the muscle activation produced by patients’ voluntary contractions.
SCHEDULE A WEB DEMO
We’ve got a few demo formats to choose from. Choose between a simple & quick phone call, a more detailed video call, or a pre-recorded web demo.
Pick what works best for you, and we’ll take care of the rest.

DON’T JUST TAKE OUR WORD FOR IT