When first using mTrigger biofeedback, many patients ask, “Is this STIM?” From a rudimentary perspective, based on the look of the electrodes, electrode placement, and device set up, this is a reasonable question. However, at the root of their functions, neuromuscular electrical stimulation (NMES) and surface EMG biofeedback (mTrigger device) are vastly different.
What’s the Difference between NMES and sEMG biofeedback?
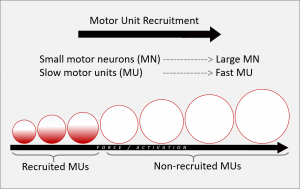
Neuromuscular electrical stimulation is used to stimulate a muscle contraction by activating the motor fibers of the muscle.(1) However, with NMES, the order in which these muscle fibers are recruited is different.(1) In normal physiologic muscle contraction, the smaller fatigue-resistant motor units are activated first, followed by larger motor units.(1) This is called Hennemann’s size principle.(2) This principle helps the muscle 1) produce an output that matches the difficultly of the task and 2) delays the onset of fatigue.(1) With NMES, a normal organized physiological muscle contraction is altered and replaced by a non-physiologic, altered muscle contraction. It was originally thought that NMES contraction was a complete reversal of Hennemann’s size principle, however, some studies are indicating that it might be more of a random/non-selective contraction order.(1) Regardless, NMES leads to a non-physiological muscle contraction that contradicts the normal highly effective unsynchronized recruitment and de-recruitment process seen in healthy muscles.
The non-physiological contraction elicited by NMES is overall much less efficient, leading to a tendency to develop neuromuscular fatigue.(1) Typically to prevent fatigue, our motor system will increase the firing rate of active motor units or simply recruit new motor units to replace the ones that are fatiguing.(2) With NMES, this isn’t an option since the muscle contraction stimulates all nerve fibers of that muscle at once.
To further emphasize this point, movements observed with NMES can be sudden, uncoordinated, and inefficient due to their non-physiological onset.(1) In contrast to the more gradual, smooth movements we are typically used to seeing during movement. Overall, NMES contractions are much less efficient than normal voluntary contraction.
Surface EMG biofeedback measures the electrical activity of the motor unit of the muscle. With biofeedback, the patient is making a strong voluntary effort to contract the target muscle. With voluntary muscle contraction, you see the correct order of recruitment of motor units from small to large diameter fibers, and encouragement of normal physiologic muscle contraction. Additionally, the activation of small, slow twitch, Type I fibers occurs first; these are the same fibers that atrophy first, and so addressing them early and often is critical to restoring muscle function.
What do the Experts Say?
For more on what Russ Paine and Mike Reinold have to say regarding NMES and sEMG biofeedback’s use in clinical practice, check out this short video.
Which One is Better?
There is a vast amount of literature in support of both sEMG biofeedback and NMES for improving muscle activation following injury or surgery.(3) However, the key is when and how long after injury/surgery you use either sEMG biofeedback or NMES.
One study comparing NMES and sEMG biofeedback found that after 6 weeks of rehabilitation, the biofeedback group demonstrated better recovery of isometric quad muscle strength and active knee extension.(4) Here is what ACL researcher and mTrigger co-founder Russ Paine says about using NMES and sEMG biofeedback: “I believe in the use of NMES if a patient is unable to make any voluntary contraction, which sometimes happens following ACL reconstruction surgery. But, once a patient is able to produce a voluntary contraction, detected by the biofeedback, we immediately switch the patient to biofeedback.”
A Patient Example
We also want to emphasize the patient experience of these two modalities, and how that impacts mental engagement and outcomes in real time.
What’s the Difference between EMG and biofeedback?
Electromyography (EMG) is a way of looking at the activity of the nerves that control the motor units of a muscle. The nerves transmit electrical signals that cause muscles to contract. With EMG we are able to see a visual representation of these signals typically as numbers or graphs. EMG is typically used by doctors to access and diagnos muscle and nerve conditions.
Biofeedback is a broad term used for a technique where information is provided back to the patient to aid in teaching them to modify or control their body in some way. This is seen, for example, in wearable devices that help to control heart rate and breathing, or in neruobiofeedback units that measure brain wave activity (EEG).
When combined, EMG and biofeedback are able to pick up the electrical signals from the muscles and have them translated in a way that can be used as visual biofeedback for the patient, encouraging them to improve their muscle contraction and movement.
Summary
There is a place for both NMES and sEMG biofeedback in rehabilitation. Understanding the physiology behind each device is essential to understanding their purpose and function. When looking to improve muscle activation and control, engage patients, and boost recovery, mTrigger biofeedback is an excellent tool to have at your fingertips.
Is Biofeedback the Right Tool?
|
Biofeedback for ACL Injuries
|
References
1. Doucet BM, Lam A, Griffin L. Focus: Biomedical Engineering Neuromuscular Electrical Stimulation for Skeletal Muscle Function. Vol 85.; 2012.
2. Mendell LM. The size principle: A rule describing the recruitment of motoneurons. J Neurophysiol. 2005;93(6):3024-3026. doi:10.1152/classicessays.00025.2005
3. Gatewood CT, Tran AA, Dragoo JL. The efficacy of post-operative devices following knee arthroscopic surgery: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25(2):501-516.
4. Draper V. Electromyographic biofeedback and recovery of quadriceps femoris muscle function following anterior cruciate ligament reconstruction. Phys Ther. 1990;70(1):11-17. doi:10.1093/PTJ/70.1.11






Leave A Comment