If we can’t see it, does it exist?
Returning to sport or high-level activity after an injury can be a challenging and difficult decision for both athletes and medical providers. Often, we seek to find the ‘best’ battery of tests to determine if and when someone is ready to take the field again.
There is a large category of injuries that lack sufficient evidence and well-studied return to sport protocols. Nevertheless, gathering information on strength, neuromuscular control, quality of movement, psychological readiness, etc. is critical for making the best prognosis and decision regarding return to play.
In the last 10 years, significant efforts have been made in research regarding return to sport testing after an ACL injury. Most recently, guidelines have concluded that although isokinetic strength testing, hop testing, and a few other ‘staple’ tests are useful, ultimately, no one test tells us everything we need to know. It is more so a combination of tests that paints a clearer picture of the situation.
Return to Sport Protocols
Although there is research to support testing after ACL injury, recent evidence has shown that strength, hop testing, and patient reported outcomes alone fail to identify who is at risk for a second ACL injury.(1) In order to best determine readiness, it is recommended that the best battery of tests should include strength testing, hop testing, psychological readiness, and a measure of quality of movement.(2,3) Furthermore, strength alone may not be enough. Deficits in rate of force development, power, and reactive strength have commonly been reported; this indicates that accessing max strength alone after an injury may not be enough.(4) When looking kinematically at how someone moves after an injury, 60% of patients demonstrated abnormal landing mechanics even though almost three quarters of them passed return to sport hop testing.(5) Furthermore, subtle but distinct differences in concentric and eccentric loading patterns between injured and non-injured sides persist 9+months after an injury.(6) Significant differences in knee flexion angle at initial contact, peak knee flexion, and knee valgus during landings were found, for example.(5) ACL research over the last several years has recommended assessing the quality of movement and a kinematic movement analysis when determining readiness for sport.(5) The bottom line is that people can cheat and compensate elsewhere providing false idea of readiness, and return to sport testing must adapt accordingly.
Physical therapists are often called ‘movement experts.’ However, what about the minute physiological adaptations and deficiencies that we cannot detect with our eyes? By putting on a critical thinking hat and accepting an assist from technology, clinicians have the ability to dissect movement on a whole new level.
Often during mid to late-stage rehabilitation, there is a drop in compliance and attention to programming details. As athletes start to get stronger and back to more ‘exciting’ activity, the persistent deficits can easily be overlooked. Furthermore, many questions persist:
– What is their deceleration capacity?
– How is their rate of force development?
– What is their ability to achieve a symmetrical peak MVC with dynamic movements?
– Do neurological deficits persist or become apparent with more dynamic and plyometric type movements?
These types of questions are difficult to answer. Typically, it requires high speed motion capture cameras, statistical analysis, and advanced programming that is not user friendly for quick clinical use. However, it is important information to know. One study even demonstrated that 53% of participants with an ACL reconstruction demonstrated deficits in rate of torque development on their surgical side.(7)
Clinical Applications
Take a look at some of the examples below. mTrigger can help to gather information and inform clinical decisions regarding return to sport readiness, strength deficits, and program/exercise progressions.
- Drop Landing
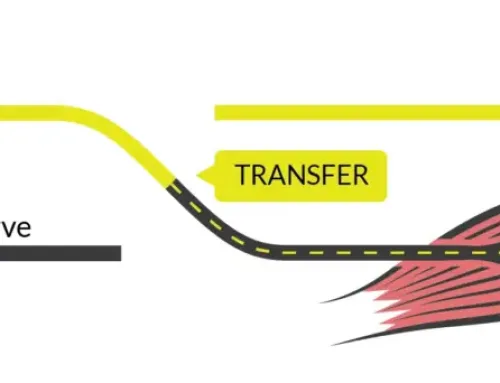
- Deceleration (running stop)
During the drop landing, the quads are required to decelerate the body and reduce forces in opposition from the ground. Even when performing a drop landing that has good form and looks “even”, there may be underlying neuromuscular firing deficits not outwardly visible. This athlete is about one year out from a major knee injury/surgery and has passed ‘typical’ return to sport testing, but her reactive EMG levels show a side to side deficit.
Follow these steps to use mTrigger surface EMG to help quantify movement quality during a drop landing:
- Begin in Settings
a. select “dual channel”
b. set the MVC based on your athlete’s strength ability (start with ~3500-4000)
c. set ‘total time’ to 7 sec (it’s a quick exercise)
d. set ‘contract’ to 5 sec
e. set ‘relax’ to 2 sec - Next, using a dual channel set up, place one channel on the left quad and the other channel on the right quad.
- When the CONTRACT period begins, instruct the patient to jump off the box with two feet and then land in a good bent knee landing position, holding for 3 seconds without moving.
- Hit ‘save session’ when the time is up (7 sec)
- Enter Track and select the most resent saved session for both channel 1 and channel 2.
- Now compare the graphs and peak MVC for each quad during landing (we aren’t focusing on average MVC in this application, just peak).
Notice for her, channel 1 is attached to her involved (left) knee and channel 2 is attached to her uninvolved (right) knee. Even though she lands with good form and evenly, there is clearly a lack of deceleration capacity and motor unit recruitment on her injured side. Despite having greater than 90% strength symmetry with isokinetic testing, there is a deficit in peak MVC that does not meet this same criterion. There is a lack of muscle activation at initial contact on the involved side. Individuals who end up sustaining a second ACL injury demonstrated a 4-fold greater asymmetry at initial contact of landing.(7)
In another example, we looked at deceleration during a running stop. This is a functional movement for any sport with quick changes in direction or cutting, and is even pertinent for something like hiking downhill when the quad is working overtime to slow down momentum. Here is another example of how you can use mTrigger to break down a movement:
- Begin in Settings
a. select “single channel”
b. set the MVC based on your athlete’s strength ability (start with ~3000-4000)
c. set ‘total time’ to 10 sec (it’s a quick exercise)
d. set ‘contract’ to 8 sec
e. set ‘relax’ to 2 sec - Next, using a single channel set up, place channel one on the involved quadriceps muscle.
- Instruct the patient to run “as quickly as possible” for 6-10 steps then stop quickly on their involved side, holding the landing for 3 seconds.
- Hit ‘save session’ when the time is up.
- Enter Track and select the most resent saved session for channel 1 and view the graph and peak MVC.
Repeat the same set up for the uninvolved side, then compare!
In this case, we see her peak MVC is relatively low, and the peak is rather small and drawn out. Now compare this to her uninvolved side and noticed how the peak is much higher and sharper indicating a faster muscle onset time and greater motor unit recruitment. This indicates that there is a lack of deceleration capacity and motor unit recruitment in the involved side that persists and needs to be addressed. These are minute details that are important when it comes to talking about sports and activities that operate in a dynamic fashion.
Now, what does this tell me clinically? This tells me there is a quadriceps peak muscle strength weakness of the involved side. It indicates that more training of the quads in the functional capacity of deceleration is needed. Although she may be “strong enough” she does not have the ability to sufficiently decelerate her center of mass and make the safe and efficient changes in direction that are predominant and necessary for her sport (lacrosse). Being able to generate a quick contraction through the quadriceps muscle is important for developing sufficient and symmetric explosive quadricep muscle strength for facilitation of safer landing mechanics.(7,8) More and more studies point towards the importance of quadriceps strength following an injury, and furthermore, its functional capacity in rate of torque development.(7,8)
For more on motor control
|
Stay up to date with our Newsletter
|
References
1. Welling W, Benjaminse A, Lemmink K, Gokeler A. Passing return to sports tests after ACL reconstruction is associated with greater likelihood for return to sport but fail to identify second injury risk. Knee. 2020;27(3):949-957. doi:10.1016/J.KNEE.2020.03.007
2. Van Melick N, Van Cingel REH, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. 2016;50(24):1506-1515. doi:10.1136/BJSPORTS-2015-095898
3. Truong LK, Mosewich AD, Holt CJ, Le CY, Miciak M, Whittaker JL. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: a scoping review. Br J Sports Med. 2020;54(19):1149-1156. doi:10.1136/BJSPORTS-2019-101206
4. Maestroni L, Read P, Turner A, Korakakis V, Papadopoulos K. Strength, rate of force development, power and reactive strength in adult male athletic populations post anterior cruciate ligament reconstruction – A systematic review and meta-analysis. Phys Ther Sport. 2021;47:91-104. doi:10.1016/J.PTSP.2020.11.024
5. Welling W, Benjaminse A, Seil R, Lemmink K, Gokeler A. Altered movement during single leg hop test after ACL reconstruction: implications to incorporate 2-D video movement analysis for hop tests. Knee Surgery, Sport Traumatol Arthrosc. 2018;26(10):3012-3019. doi:10.1007/S00167-018-4893-7/FIGURES/3
6. Read PJ, Michael Auliffe S, Wilson MG, Graham-Smith P. Lower Limb Kinetic Asymmetries in Professional Soccer Players With and Without Anterior Cruciate Ligament Reconstruction: Nine Months Is Not Enough Time to Restore “Functional” Symmetry or Return to Performance. Am J Sports Med. 2020;48(6):1365-1373. doi:10.1177/0363546520912218
7. Huang Y-L, S Mulligan CM, Johnson ST, et al. Explosive Quadriceps Strength Symmetry and Landing Mechanics Limb Symmetry After Anterior Cruciate Ligament Reconstruction in Females. J Athl Train. 2021;56(8):912-921. doi:10.4085/351-20
8. Schmitt LC, Paterno M V., Ford KR, Myer GD, Hewett TE. Strength Asymmetry and Landing Mechanics at Return to Sport after ACL Reconstruction. Med Sci Sports Exerc. 2015;47(7):1426. doi:10.1249/MSS.0000000000000560






Leave A Comment