Author: Mallory McFarlane, DPT of Dry Creek Physical Therapy, Utah
Check out Instagram for more from Dr. McFarlane and Dry Creek PT!
In my clinic, I work with elite high school, collegiate, and professional athletes. One of the athletic populations I routinely work with are elite gymnasts. Gymnasts put a great deal of strain on their bodies while they are accomplishing incredible feats. However, because of the repetitive strain, they often get injured.
I have been successfully using mTrigger biofeedback for about two years with these (and other) patients. It is a versatile device that can be used for many different muscle groups. I mostly use mTrigger to help patients and athletes increase activation of a particular muscle group. However, you can also use the device to relax or inhibit a particular muscle group.
One of the injuries that I see a lot in gymnasts is fractures at the pars interarticularis (“pars fractures”) in the lumbar spine. This diagnosis is also referred to as spondylolysis. Pars fractures occur from repetitive and excessive extension.
Fortunately, there are things that we can do to minimize the risk of pars fractures in gymnasts and other athletes. A thorough evaluation of the athlete can help determine the cause of low back pain before it progresses to a pars fracture. The evaluation can help discover such causes as muscle imbalances, flexibility deficits, and movement impairments.
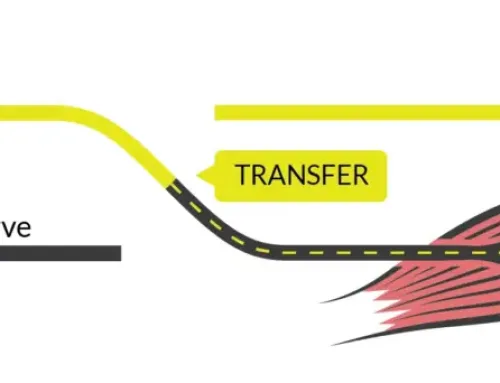
One impairment that I typically see in gymnasts with low back pain and spondylolysis is an overactivation of the lumbar paraspinals and decreased strength and activation of the gluteus maximus. Both the lumbar paraspinals and gluteus maximus muscles are muscles that extend. Often, these athletes have difficulty differentiating activation between the two extensor muscles. Weak gluteals will often cause a compensation of the lumbar paraspinals to help make up for the lack of gluteal strength.
Overactivation and compensation of the lumbar paraspinals can cause an increase in low back pain and can lead to increased strain at the lumbar spine, leading to spondylolysis. This is where mTrigger becomes an essential rehab tool for these patients.
How to use mTrigger to decrease lumbar paraspinal overactivation:
1. Place the electrodes at the lumbar paraspinals. Use dual channel – one pair on the right and one pair on the left paraspinals.
2. Instruct patient to perform resisted trunk extension to determine the MVC goal setting for maximum lumbar paraspinal activation.
3. With mTrigger in place, instruct patient to start performing simple hip extension exercises.
Examples include: double leg bridges, kneeling hip hinging, prone and quadruped hip extension
4. As the patient performs hip extension exercises, instruct them to keep the lumbar activation low. As they extend their hip, the muscle activation meter attached to the lumbar paraspinals should not drastically increase. If the meter does increase, the patient can see it and immediately make the change in the way they are performing the exercise.
NOTE: You can also use dual channel mode to simultaneously measure activation of paraspinals and glutes to encourage activation of the glute med while maintaining low activation of the paraspinals.
5. As the patient makes improvements in the quality of movement of simple hip extension exercises, you can progress them to more complex exercises.
Examples include: single leg bridges, deadlifts, single leg RDLs, and step ups
Patients who use mTrigger in this way help to improve neuromuscular control over their hip extensor muscles through visual biofeedback. As the patients learn to properly use their glutes, they can more effectively strengthen them without putting excessive strain through the lumbar spine. This, in turn, will help to decrease the risk of spondylosis and low back pain in gymnasts and other athletes.
mTrigger has been a very effective rehab tool in my clinic and for my athletes. It is crucial to select the right exercises that will be most effective for your patient, and it is equally as important that the patient does the exercises correctly and uses the right muscles without compensation. It is challenging to see muscle compensations with the naked eye. mTrigger can help you see these compensation patterns more clearly in your patient and give them the feedback to make the necessary changes.
As gymnasts and other athletes apply these principles to simple and complex exercises in the gym or clinic, they will be able to learn how to properly use their glutes vs. lumbar paraspinals. Motor learning by use of biofeedback will help the patient perform their sport utilizing the correct muscles and decrease their risk of overuse injury.
Photo Credit: https://www.sportsinjurybulletin.com/lumbar-spondylolysis-in-adolescent-athletes-breaking-the-curse/







When you do the resisted trunk extension to determine the MVC goal setting for maximum lumbar paraspinal activation do you sent the MVC goal below that then or at a certain percentage? I guess I figure you want their extensors to be a whole lot quieter during the bridge than when they are doing a resisted extension.
Hi Amanda, great question. Even though they are aiming for minimal activation of the lumbar paraspinals, setting the goal this way can help the patient understand their activation level in relation to their maximum. Once they gain some control, you can reduce the goal so the app shows even smaller amounts of activation, helping the patient to activate less and less over time. This is inverse to how you would increase the goal as a patient gains strength. However, you can absolutely set the goal lower than max from the get-go if that resonates better with you and your patients!